HORMONAL MALE AXIS AND HORMONES BLOODWORK
The hormonal axis is a conjunction of hormones, enzymes, and releasing factors that together function to maintain the production of testosterone, estradiol, spermatozoa, and other hormones fundamental for male survival, well-being, reproductive functions, muscle strength, bone density, and psychological stability.
This axis is affected by many factors such as obesity, which causes an increase in the conversion of testosterone to estradiol, or stress, which directly reduces testosterone. It is also affected by various medications, including testosterone and its derivatives, which inhibit this axis through negative feedback. This means that if we increase androgens, the production of testosterone will be suppressed.
2. WHAT IS THE MALE HORMONAL AXIS?
When analyzing a man's hormonal profile, we first focus on the hormonal axis and all the factors that affect it. These factors reveal the current endogenous production of certain hormones and others that intervene, delineating the balance of current therapy.
They also provide information regarding fertility, but for more in-depth analysis, a semen analysis would be necessary.
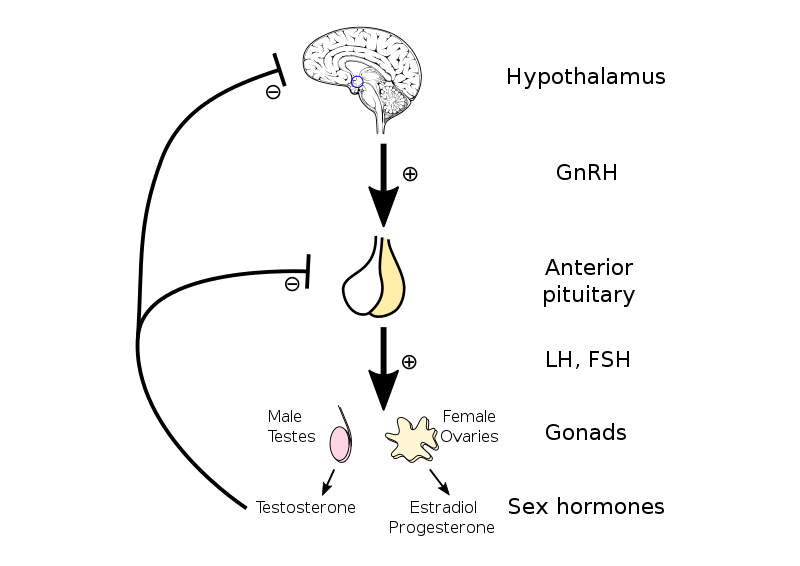
The hypothalamus is the hormonal center of the brain along with the pituitary gland. It is regulated by negative feedback; higher levels of certain hormones such as androgens, testosterone, estradiol, progesterone, and prolactin reduce the endogenous production of testosterone and some of its metabolites.
The basic function is that the hypothalamus releases a releasing factor, GnRH, which stimulates the anterior pituitary to produce LH and FSH. These gonadotropins go to the Leydig cells in the testes to produce testosterone (via LH) and to the seminiferous glands to produce sperm (via FSH).
In summary, this is known as the hypothalamic-pituitary-gonadal axis or the male hormonal axis.
3. ANALYTICS OF THE MALE HORMONAL AXIS
Now we will look at a series of analytes that are very important in a male. These will provide extensive information about the current endogenous production of testosterone and all its metabolites.
It is essential to perform the test while fasting, at a biochemical laboratory, or a private medical center, as many of the values needed are not typically provided by public health services without specific indications.
We will look at the analytes that should be sought in a man, their normal values, which are physiologically normal, and their ranges. We will also provide explanations of what each one means and some additional interesting data that offer a lot of useful information.
- TOTAL TESTOSTERONE
Testosterone is the androgen primarily produced by the testes in the Leydig cells under the influence of luteinizing hormone (LH).
It is responsible for secondary sexual characteristics and the regulation of sexual desire (more due to DHT), muscle mass, and bone density, from which most anabolic capacity originates.
However, the majority of total testosterone, between 60-70%, binds to Sex Hormone-Binding Globulin (SHBG) and becomes unavailable to produce any physiological effect in the tissues.
Another 30-38% is bound to Albumin, which is not entirely inactive because Albumin binding is weak and reversible, so this fraction can dissociate and become free testosterone.
Additionally, on average, about 1% of testosterone, via the enzyme Alpha Aromatase, is converted into Estradiol, leaving about 2% of free testosterone, which is what really exerts the anabolic potential and other physiological functions.
Total testosterone values in men vary between laboratories and are subdivided by age:
-Age 19-39 years: 300-1000 ng/dL
-Age 40-59 years: 300-800 ng/dL
-Age 60 years and older: 300-700 ng/dL
Above these levels, which are considered normal, there may be an anomaly that could range from tumors in the hypothalamus, with an overproduction of GNRH, or it could be caused, as may be your case, by the use of exogenous testosterone.
Below this level, we have primary hypogonadism if the reasons are genetic, or secondary hypogonadism if it is acquired due to some disease, lifestyle, or drug use.
As we see, values differ by age ranges, and there is an explanation for this:
The decrease in testosterone levels with age, known as andropause or late-onset hypogonadism, is due to several physiological factors affecting both Leydig cells in the testes and the hypothalamic-pituitary-testicular axis.
This occurs at both the pituitary-hypothalamic level and at the level of the testes and SHBG:
-With age, Leydig cells become less sensitive to LH, resulting in reduced testosterone production.
-The capacity of Leydig cells to produce testosterone in response to hormonal stimulation decreases.
-The number of Leydig cells may decrease with age, reducing the total capacity of the testicle to produce testosterone.
-Leydig cells can suffer damage from oxidative stress and accumulation of metabolic waste products, negatively affecting their function.

-The hypothalamus may produce less GnRH with age, leading to less stimulation of the pituitary to release LH and FSH.
-The pituitary may release less LH and FSH in response to GnRH, decreasing the stimulation of Leydig cells and thereby reducing testosterone production.
-The negative feedback between testosterone levels and the production of GnRH and LH may become less efficient, altering hormonal regulation.
-Additionally, SHBG levels may increase, leading to a lower amount of free and bioavailable testosterone.
-Aromatase enzyme activity may increase with age, converting more testosterone into estrogens, reducing testosterone levels.
-Chronic conditions like obesity, type 2 diabetes, cardiovascular diseases, and other health problems can contribute to the decrease in testosterone levels.
-LUTEINIZING HORMONE (LH):
LH is secreted by the anterior pituitary gland in response to GNRH and stimulates the production of testosterone in the Leydig cells in the testes.
It is the primary gonadotropin responsible for testosterone production and is the most important factor in evaluating the recovery of the hormonal axis.
All androgens, without exception, inhibit this axis and progressively reduce LH secretion by the hypothalamus or anterior pituitary.
-Adults: 1.8 - 8.6 IU/L (international units per liter)
Below this amount, it is considered hypogonadism. If it is caused by testosterone or its derivatives, it is reversible, but with repeated use, the response of Leydig cells will worsen due to their cell death, which occurs more at very high doses, and there is also a loss of sensitivity in the anterior pituitary to secrete LH, both due to dose and duration of exogenous androgen use.
The two factors that limit the inhibition of the axis are dose and time. Higher doses make axis recovery more difficult, and the longer the use, the same applies.
When we elevate LH through analogs like Ovitrelle or HCG, which is basically an LH mimetic, or with Clomiphene or Enclomiphene, to assess the recovery of the axis, we must interrupt the protocol with LH.
That is, if we want to know exactly how our axis recovery has been so far and we are in a post-cycle process with HCG or SERMs, we must stop the treatment before doing the analysis.
-FOLLICLE-STIMULATING HORMONE (FSH):
FSH, also secreted by the anterior pituitary gland, is essential for spermatogenesis in the testes. It primarily stimulates the seminiferous tubules to produce sperm.
-FSH in adult men: 1.5 to 12.4 mIU/mL (milli-international units per milliliter)
It is not as interesting regarding testosterone production, but it gives us information on how the hormonal axis recovery is progressing and especially on fertility.
Within spermatogenesis, FSH has very important functions:
FSH is fundamental for the production and maturation of sperm. It acts directly on Sertoli cells in the testes, stimulating them to support sperm production.
Sertoli cells, when stimulated by FSH, produce nutrients and growth factors necessary for the development and maturation of sperm.
Sertoli cells also produce inhibin B in response to FSH, which provides negative feedback to the pituitary gland to regulate FSH secretion and maintain hormonal balance.
FSH helps in the development and maintenance of seminiferous tubules, which are the sites within the testes where spermatogenesis occurs.
These tubules are essential for sperm production and the transport of immature sperm to the epididymis, where they fully mature.
-PROLACTIN (PRL):
Secreted by the anterior pituitary gland, elevated prolactin levels can inhibit GnRH secretion, which in turn can decrease LH and FSH levels, affecting testosterone and sperm production.
-Prolactin in adult men: 2 to 18 ng/mL (nanograms per milliliter)
It is important to know that estradiol increases prolactin, and these prolactin elevations observed when using nandrolones are often actually exacerbated estradiol elevations.
ESTRADIOL (E2):
Although it is predominantly a female hormone, estradiol is also present in men and is produced through the conversion of testosterone, known as aromatization.
It is important to emphasize that the best way to request this testosterone metabolite is as Ultrasensitive Estradiol.
It is crucial for regulating bone metabolism and sexual function.
-10 to 40 pg/mL (picograms per milliliter)
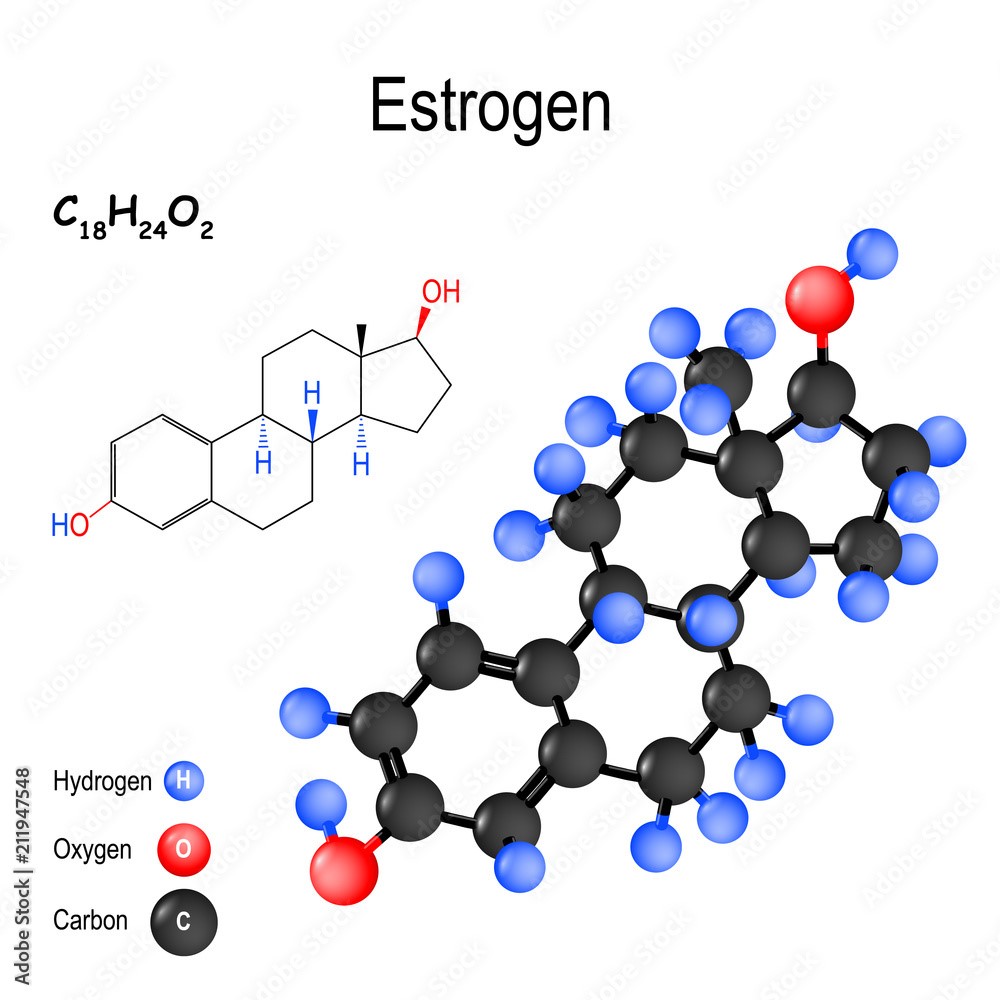
Excess testosterone increases the amount of this hormone, and this excess has unpleasant health consequences, such as gynecomastia, increased blood pressure, sweating, impotence, etc.
Estradiol contributes to the regulation of sexual desire. Inadequate levels can negatively affect male libido, both in excess and deficiency.
Along with testosterone, estradiol helps maintain erectile function and overall sexual health.
Estradiol is crucial for maintaining bone density in men. Low levels can lead to greater susceptibility to osteoporosis and bone fractures.
Estradiol has cardioprotective effects, including improving endothelial function, reducing vascular inflammation, and contributing to blood pressure regulation.
Adequate estradiol levels are associated with better mood and cognitive functions, such as memory and concentration.
-SEX HORMONE-BINDING GLOBULIN (SHBG):
SHBG binds to sex hormones like testosterone and estradiol, regulating their bioavailability. SHBG levels can influence the amount of free testosterone available.
All steroids reduce SHBG, especially DHT derivatives, leaving more free testosterone to exert its anabolic actions.
The lower the SHBG, the higher the proportion of free testosterone capable of exerting physiological functions.
-10 to 57 nmol/L (nanomoles per liter)
-DEHYDROEPIANDROSTERONE SULFATE (DHEA-S):
Produced by the adrenal glands, DHEA-S is a precursor to sex hormones and plays roles in immune function and energy production.
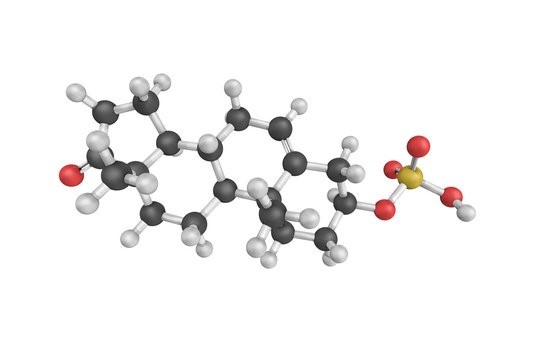
-Ages 20-29: 138.5-475.2 µg/dL
-Ages 30-39: 120.8-486.9 µg/dL
-Ages 40-49: 95.4-446.4 µg/dL
-Ages 50-59: 70.2-395.6 µg/dL
-Ages 60-69: 42.8-329.1 µg/dL
-Ages 70-79: 31.6-224.6 µg/dL
DIHYDROTESTOSTERONE (DHT):
DHT, or dihydrotestosterone, is an androgen, a male sex hormone derived from testosterone through the action of the enzyme alpha-reductase.
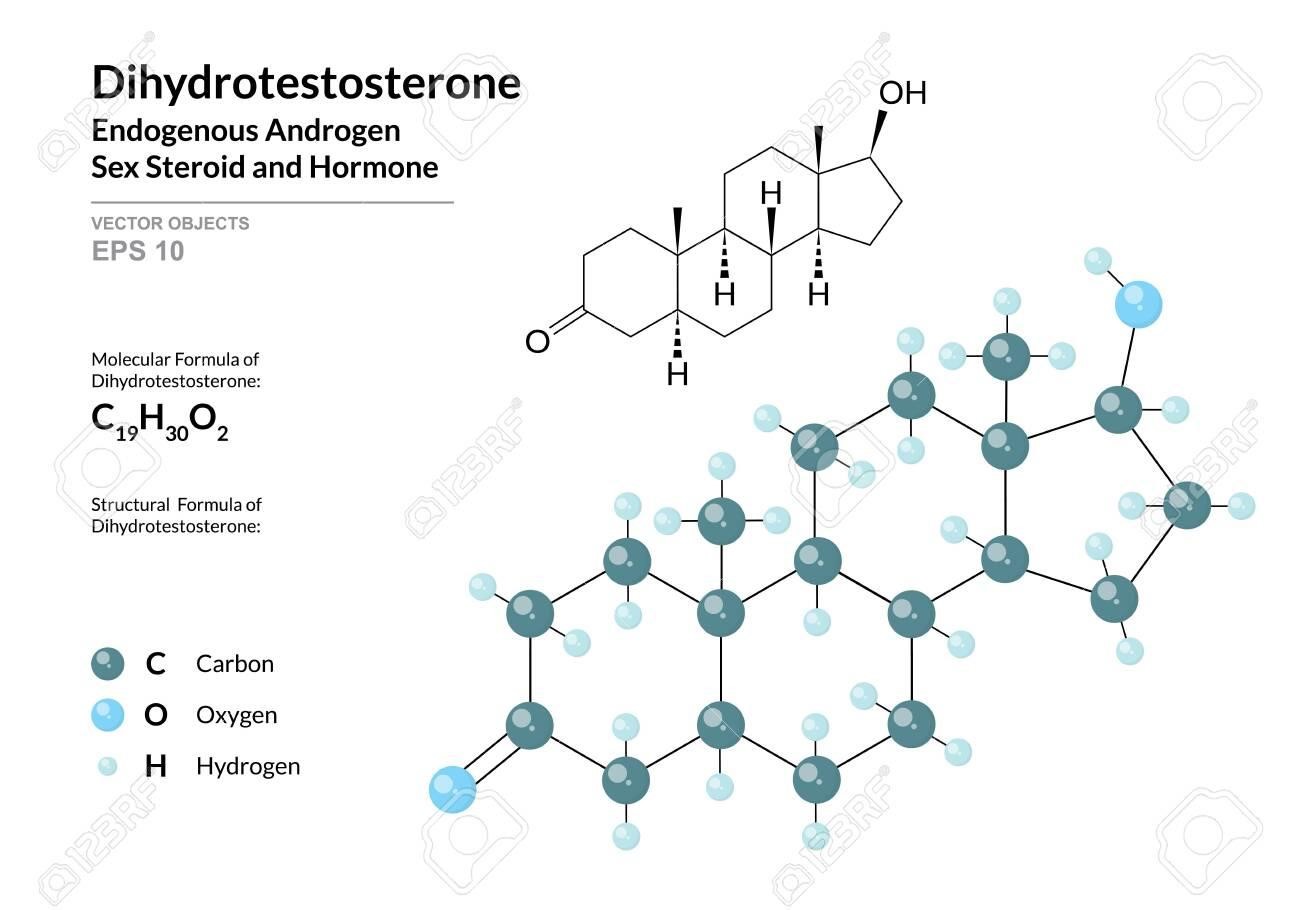
It is one of the most potent hormones in the human body and plays a crucial role in developing male characteristics, such as facial and body hair growth, genital development, and voice deepening during puberty.
DHT is also responsible for strength enhancement through its action on the nervous system and virilization in women.
In men, no anabolic steroid elevates DHT other than simple testosterone, and it has very important physiological functions as it is among the most important psychologically.
It is important to note that although DHT is a strong androgen, it does not have anabolic capacity because an enzyme called 3-Hydroxysteroid dehydrogenase literally inhibits its actions in skeletal muscle.
-Normal range: 30 - 850 ng/dL (nanograms per deciliter)
-FREE TESTOSTERONE:
Free testosterone is the fraction of testosterone in the body not bound to carrier proteins in the blood, such as sex hormone-binding globulin (SHBG) or albumin.
It represents a small portion of the total testosterone in the body, but it is biologically active and capable of entering cells to exert its physiological effects.
-Normal range: 5 - 21 ng/dL (nanograms per deciliter)
High doses of testosterone and other androgens leave more free testosterone that can exert its anabolic actions.
CONCLUSION
The male hormonal axis, as well as its balance in metabolites, is fundamental for development within bodybuilding and fitness, as it will determine both the prevention of adverse effects and the good psychological and sexual status of the male.
In this article, we have covered many aspects; remember that values can vary between laboratories and the measurement units of each parameter, so guide yourself by the upper and lower limits.
Remember that all AAs and SARMs inhibit the axis without exception, and if endogenous production is to be recovered, the use of these must be interrupted and usually followed by a Post Cycle Therapy (PCT) protocol.
In future articles, we will see what a post cycle is, how to perform it correctly, and the different types of post cycle protocols.
Remember that you can leave your suggestions for future articles in the support email.
Nutribuilder
Julio Vizuete Velasco
Educator on PEDs and health and Bodybuilding Coach