17 Apr
Blood analysis during steroids use

1. Introduction
When considering using steroids, we often think about associated health problems like gynecomastia, alopecia, acne... all aesthetic adverse effects that are visible at first glance. However, few people truly worry about what can really ruin your life: organic adverse effects.
But how can we know if these health problems are occurring? Blood tests are the most direct, simple way to prevent steroid side effects before they develop or to detect them as they develop and to what extent, seeking actions through modification of supplementation, drugs, habits, or diet to improve these parameters.
2. What should we consider when using steroids
Once we start using steroids, we must be prepared to suffer adverse effects of all kinds, but obviously, there are different ways of consuming them.
One can use them in an uncontrolled and terrible manner, from which beneficial effects may not be achieved, and furthermore, more side effects than expected for the dose and drugs involved.
As for blood tests, they are not the same for a healthy person as for someone using anabolic steroids. We all agree on that, but there are doubts about when these tests should be done and what we should expect.
What do I mean by this? Blood tests are commonly done before and after consumption, which is a big mistake. You perform tests when your body is completely free of external agents and you do it again when you are no longer using any compound or perhaps you are starting the post-cycle phase, which is an error.
3. How to correctly do a blood test
Blood tests should not be an excuse to continue using steroids; rather, they should be used to predict undesirable adverse effects, anticipate them, and see "the crap" as soon as possible.
Therefore, I propose a different model:
- Blood test prior to use
- Blood test at 4 weeks of use
- Blood test after 4-6 more weeks of use and if possible, with a change in preparation, with another compound, or perhaps with a change in dose or adjustment
- Blood test prior to finishing the cycle or blast
- Blood test after 4 weeks of finishing the cycle or blast
They may seem like a lot, but the amount of information they provide is incredible because we have:
- Health markers of the organism naturally
- Health markers after starting the use of substances and the first response
- Health markers after several weeks using substances and making increases and/or changes of substances
- Health markers after several weeks of stopping the drugs/initiating PCT/TRT
Once we know how to schedule these analyses, we should know what we are going to analyze and why, because perhaps we need some values that are not so common and are really useful for our blood test to truly reflect what is happening in the body and not just be a "Okay bro, continue with the cycle".
It's important to be fasting, not having had a heavy meal the day before, no cheat meals or anything similar, as that can skew several values from reality.
4. Hormonal profile
The hormonal profile is a group of hormones and markers that will give us information about the current situation of the hypothalamic-pituitary-gonadal axis, the axis that connects the brain, testicles, and finally, how the natural secretion of testosterone is currently.
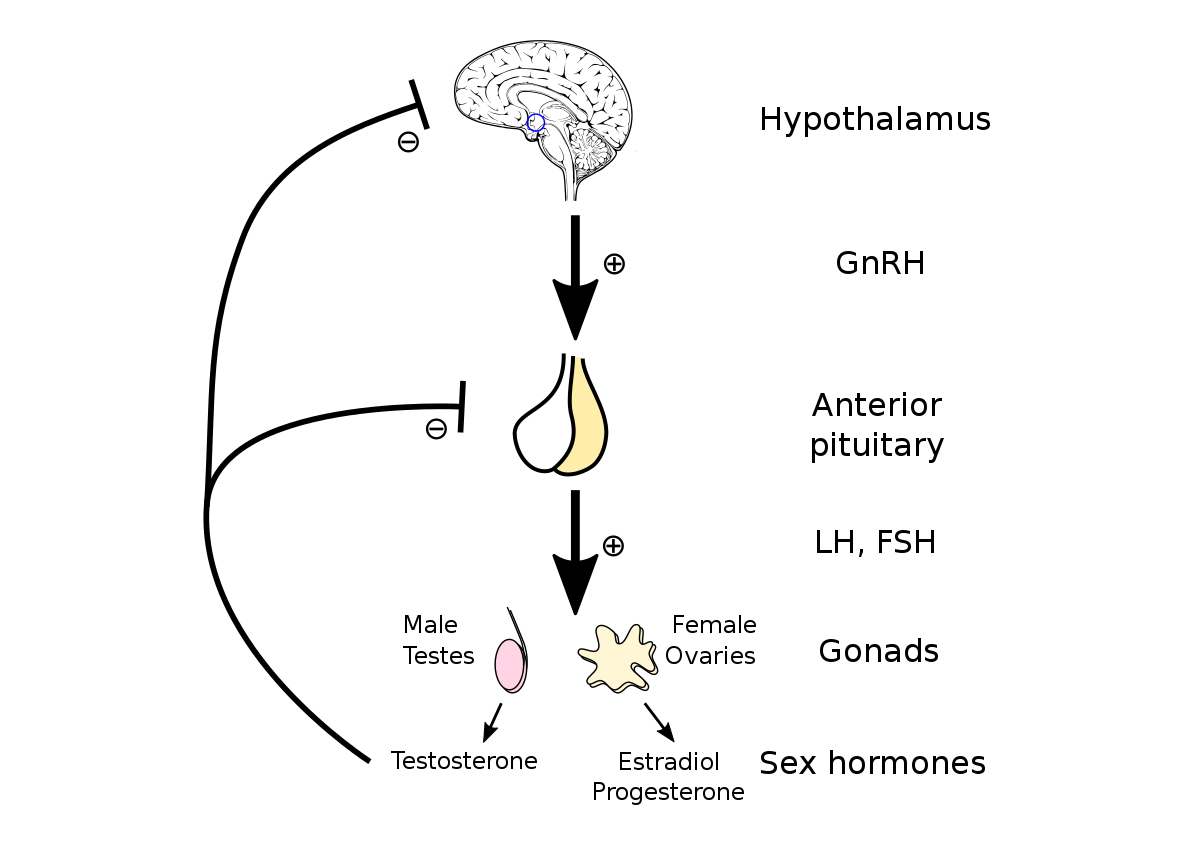
Repeated use of anabolic steroids generates a double atrophy, first at the hypothalamic level (in the brain), which recovers over time after stopping the drugs, and then at the testicular level, which is different and can recover to a greater or lesser extent, as high doses and continuous periods of use of AAS result in cell death in Leydig cells, which produce testosterone in the testicle.
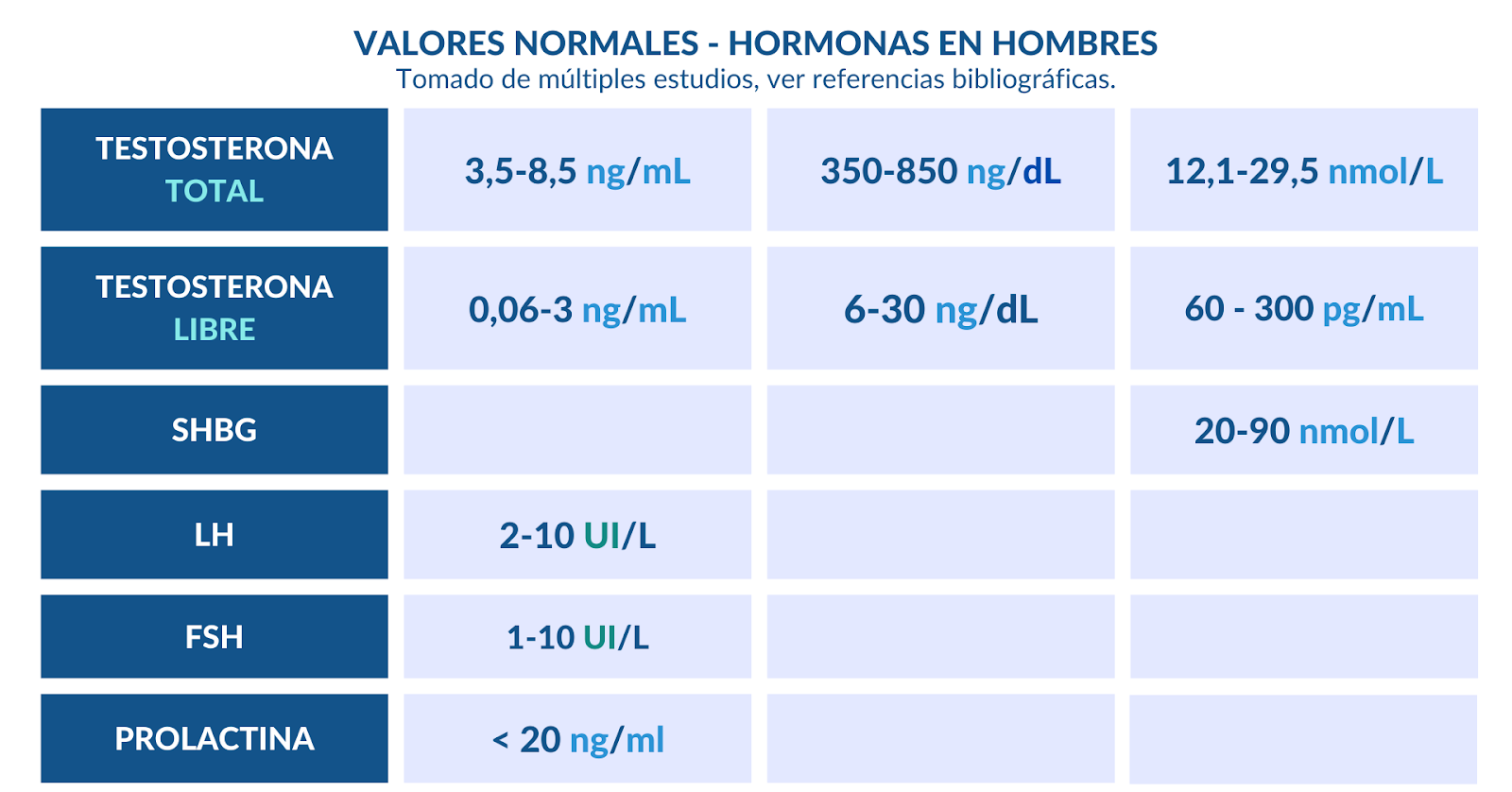
Therefore, we will measure LH and FSH, which are two hormones that signal testosterone secretion, to see how the hypothalamus is responding.
Total Testosterone, to know how the testicle is responding, and Free Testosterone, to know the fraction that is not bound to plasma proteins.
SHBG, to know how much testosterone will bind to this globulin, which will not be free. Interestingly, most steroids reduce DHT and especially DHT derivatives.
Estradiol, a hormone we talked about in the previous article, to see if the aromatization of testosterone to estrogen is correct.
Prolactin, which is a hormone that in men can be elevated by certain compounds in the preparation like Trenbolone and Nandrolone, or in cases of excessive stress.
5. Hepato-biliary profile
The liver is a vital organ responsible for detoxifying the body, alcohol, and drugs.
We should not only talk about the liver but also about the liver-gallbladder-pancreas complex, which is a complex of organs that is responsible for many functions such as cholesterol formation, fat digestion, control in part of certain nutrients, and as we have mentioned, detox function.
We will look at liver enzymes, ALT, GGT, and AST, which will indicate how the liver tissue is finally, if there is stress, injury, or even a degree of fibrosis.
This would mainly be the main metric to evaluate the status of the liver under the use of oral steroids, but also under excessive stress through the consumption of other drugs or very intense exercise.
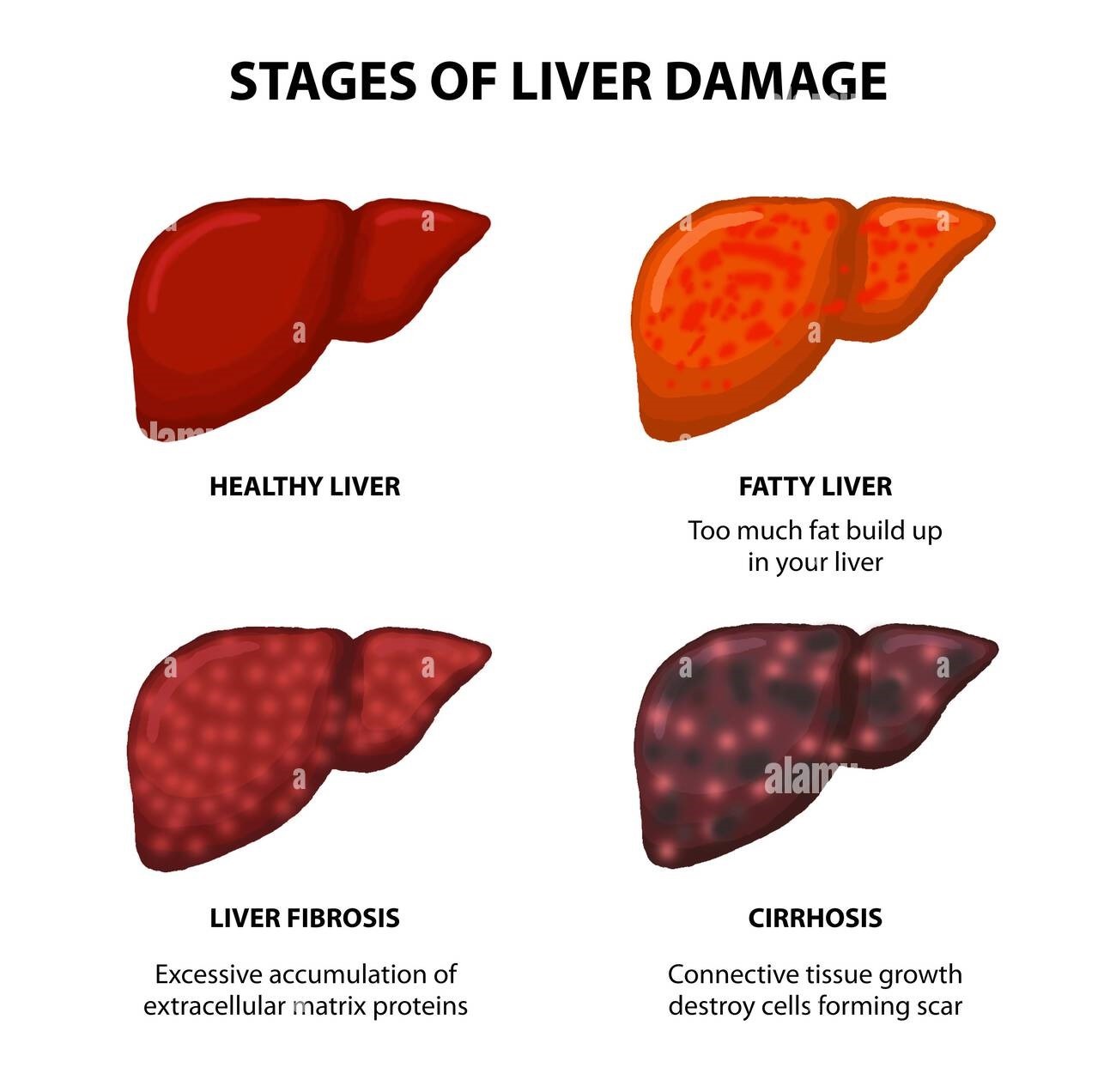
Values can be skewed if we have not rested from training 48-72 hours prior, which is essential to properly evaluate this test and have a complete and truthful view of liver function.
6.Red Blood Cell Profile
The Red Blood Cell Profile is a set of components found in the blood, mainly concerning the quantity, size, and concentration of red blood cells, as well as their iron content.
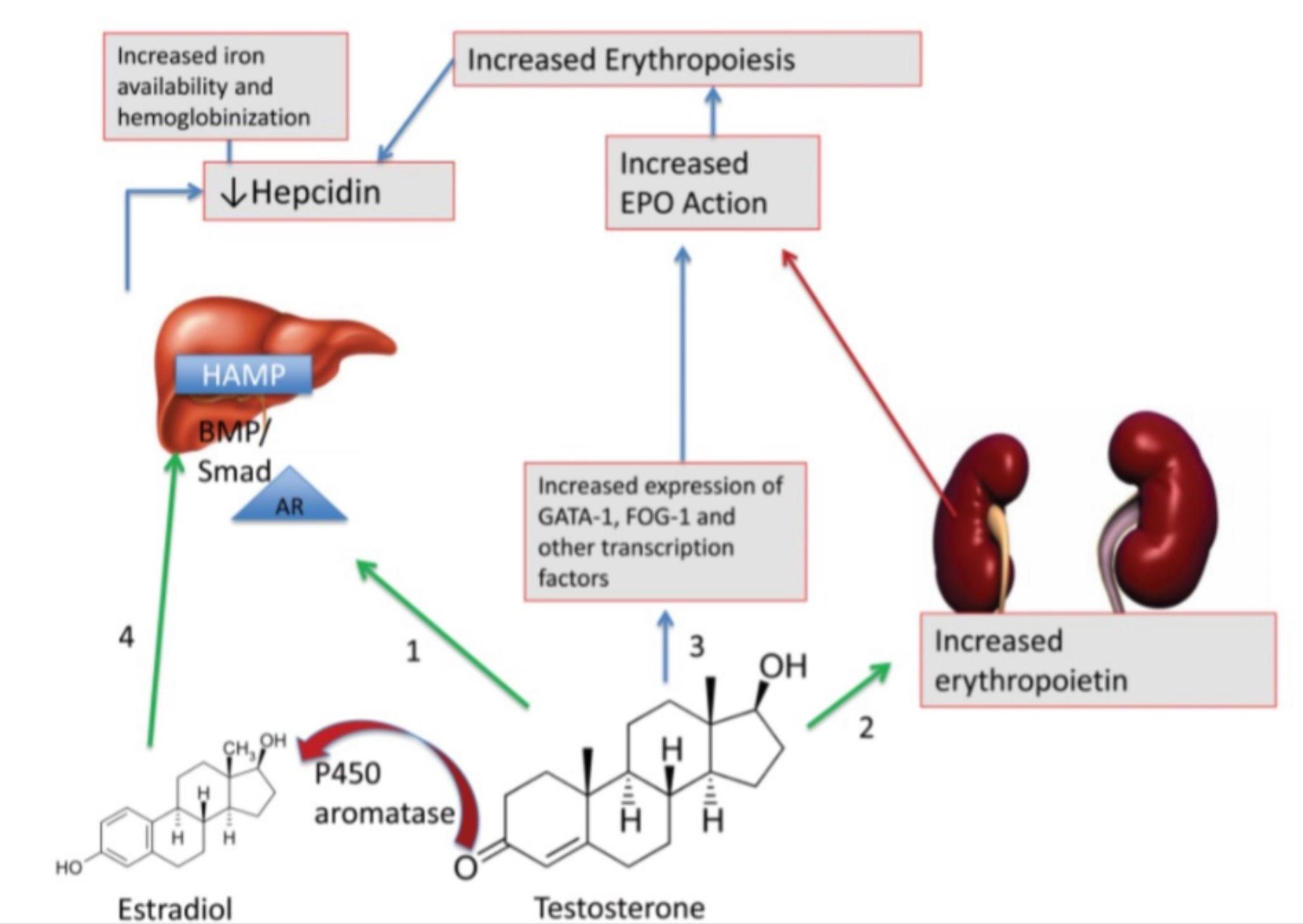
This profile is particularly relevant for pharmacology users as the use of anabolic steroids can increase erythrocytosis, resulting in a condition called Polycythemia, which entails an excessive accumulation of red blood cells in the blood, significantly elevating the risk of thrombosis, blood clots, and cardiovascular accidents.
-Red Blood Cell Count (RBC) or Hematocrit: This number indicates the quantity of red blood cells present in a blood sample. Abnormal values may indicate anemia (if low) or polycythemia if high:
4.1-5.75.
-Hematocrit (HCT): This value represents the percentage of red blood cell volume compared to the total blood volume. A high hematocrit may indicate dehydration or polycythemia, while a low one may indicate anemia or blood loss:
Men: 39% to 50%.
Women: 34% to 44%.
-Hemoglobin (Hb): Hemoglobin is a protein in red blood cells that transports oxygen. Its level can indicate the blood's capacity to carry oxygen. Low values may indicate anemia:
Men: 13.8 to 17.2 g/dL.
Women: 12.1 to 15.1 g/dL.
-Mean Corpuscular Volume (MCV): This parameter indicates the average size of red blood cells. It can help determine the specific type of anemia if present:
80 to 100 fL (femtoliters)
-Mean Corpuscular Hemoglobin Concentration (MCHC): This value indicates the concentration of hemoglobin in a given volume of red blood cells. It can help differentiate between different types of anemia:
31.5-36 g/dL
-Red Cell Distribution Width (RDW): This term refers to the variability in the size of red blood cells. It can indicate certain medical conditions, such as nutritional deficiencies or chronic diseases:
11.5-15.5%.
These values may vary between laboratories or the units of measurement of each analyte.
It is important to drink enough water the day before the analysis, urinate before extraction, and not drink excessive water as it could skew the values.
7.Lipid and Inflammatory Profile
The lipid profile is a set of analytes that reflects the behavior of all lipids and cholesterol, not just analyzing cholesterol but all the lipoproteins involved in its transport.
It is the most important analytical group for assessing cardiovascular risk, usually requested along with some other value reflecting tissue inflammation.

There is much controversy regarding the actual importance of some of the values, such as the analytical importance of HDL, a fraction of lipoproteins that has always been thought to have a "protective" role in cardiovascular health. However, recent medical guidelines have discarded this supposed role, concluding that higher HDL levels are not related to a lower incidence of cardiovascular risk.
The conclusion is that the lower the total cholesterol (CT) and LDL, especially, the lower the mortality rate, and the objective should be to maintain each fraction below certain values.
But one premise is certain, "the lower, the lower the risk of cardiovascular disease."
-Total Cholesterol: Reflects the amount of cholesterol in the bloodstream, summing all its fractions, expressed in mg/dl.
Normal range: <200 mg/dl but ideally below 150 mg/dl.
-LDL Cholesterol: A lipoprotein that is heavily laden with cholesterol and is considered "bad cholesterol." We should aim to have it "as low as possible." This fraction accumulates in the endothelium or vascular walls, along with other particles like foam cells and dead cells, forming the atheroma plaque, the main cause of atherosclerosis.
Normal range: <100 mg/dl but ideally below 70 mg/dl.
-HDL Cholesterol: A lipoprotein with a large protein component and low lipid content. As mentioned, its value is not particularly relevant. It can also be falsely elevated by alcohol consumption due to a subunit called HDL3.
It is concluded that there should be at least 40 mg/dl of this lipoprotein in the blood, but it is discarded because the atherogenic coefficient (LDL/HDL) is an irrelevant analytical value that does not reflect cardiovascular risk.
-Triglycerides (TG): Triglycerides are the form chosen by nature to store energy as fat in our adipose cells. Therefore, an excess presence of them in the blood can contribute to a higher cardiovascular risk.
Desirable: <150 mg/dl.
At this point, it would be sufficient for a healthy individual. However, if we want to know more about our lipid profile analysis and/or are users of steroids, then we will dig deeper.
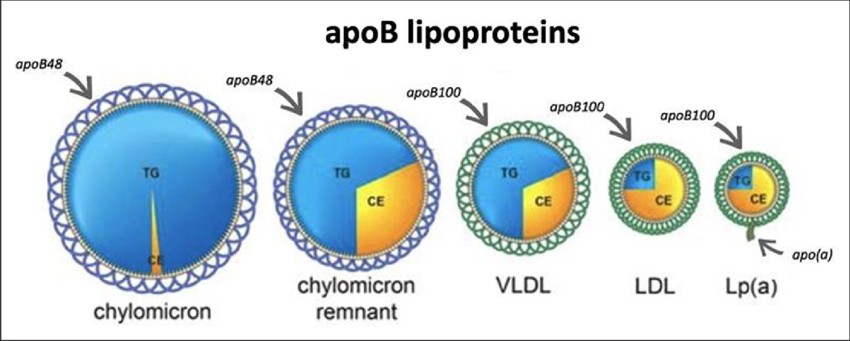
There is a protein fraction in lipoproteins that can provide a lot of information about how these lipoproteins behave, such as:
-Apolipoprotein B (ApoB): It is the protein fraction of LDL, and if elevated, it indicates whether it is being accumulated or deposited in blood vessels.
The target is to have an ApoB quantity of <90 mg/dl, with 50 mg/150 mg being the normal values.
In addition to the total cholesterol, LDL, and ApoB quantities, if the individual has a high cardiovascular risk, inflammation is one of the most important values to determine if there is cardiovascular risk.
There are two values to determine tissue inflammation: high-sensitivity C-reactive protein (hs-CRP) and homocysteine.
-High-Sensitivity C-Reactive Protein (hs-CRP): It is an analyte that reflects tissue inflammation but with higher sensitivity, leaving aside typical inflammatory processes of common diseases, heavy weight training, and others, which involve inflammation per se.
Desirable values are <1 mg/L.
-Homocysteine: Homocysteine is an amino acid obtained from the metabolism of methionine. It is elevated especially when there is inflammation and can be elevated by excessive consumption of red meat in the diet, which contains a high amount of this amino acid.
Desirable values are <8 μmol/L.
8.Renal profile
The kidney is the organ that should concern us the most along with the heart when talking about organic effects, which is why I wanted to leave it for last.
The long-term use of anabolic steroids, especially at high doses, leads to a loss of renal function, especially if appropriate prophylactic measures are not taken.
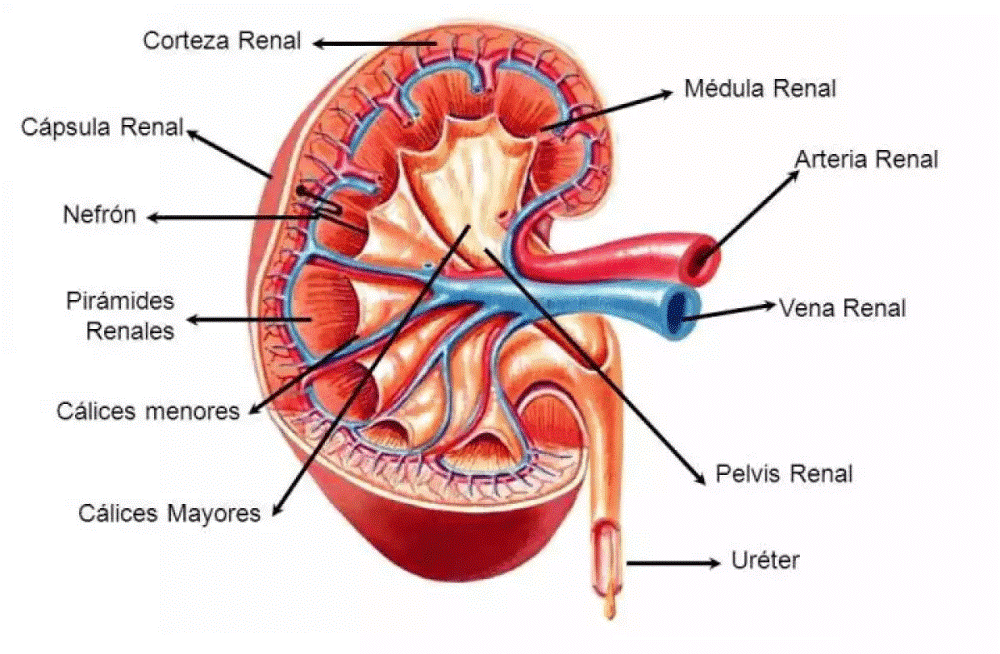
Regarding the analytical values that we are going to take into account in a blood test to determine renal function, it is worth noting that a 24-hour urine test provides even more information, but today we will only see the values that we can see in the blood.
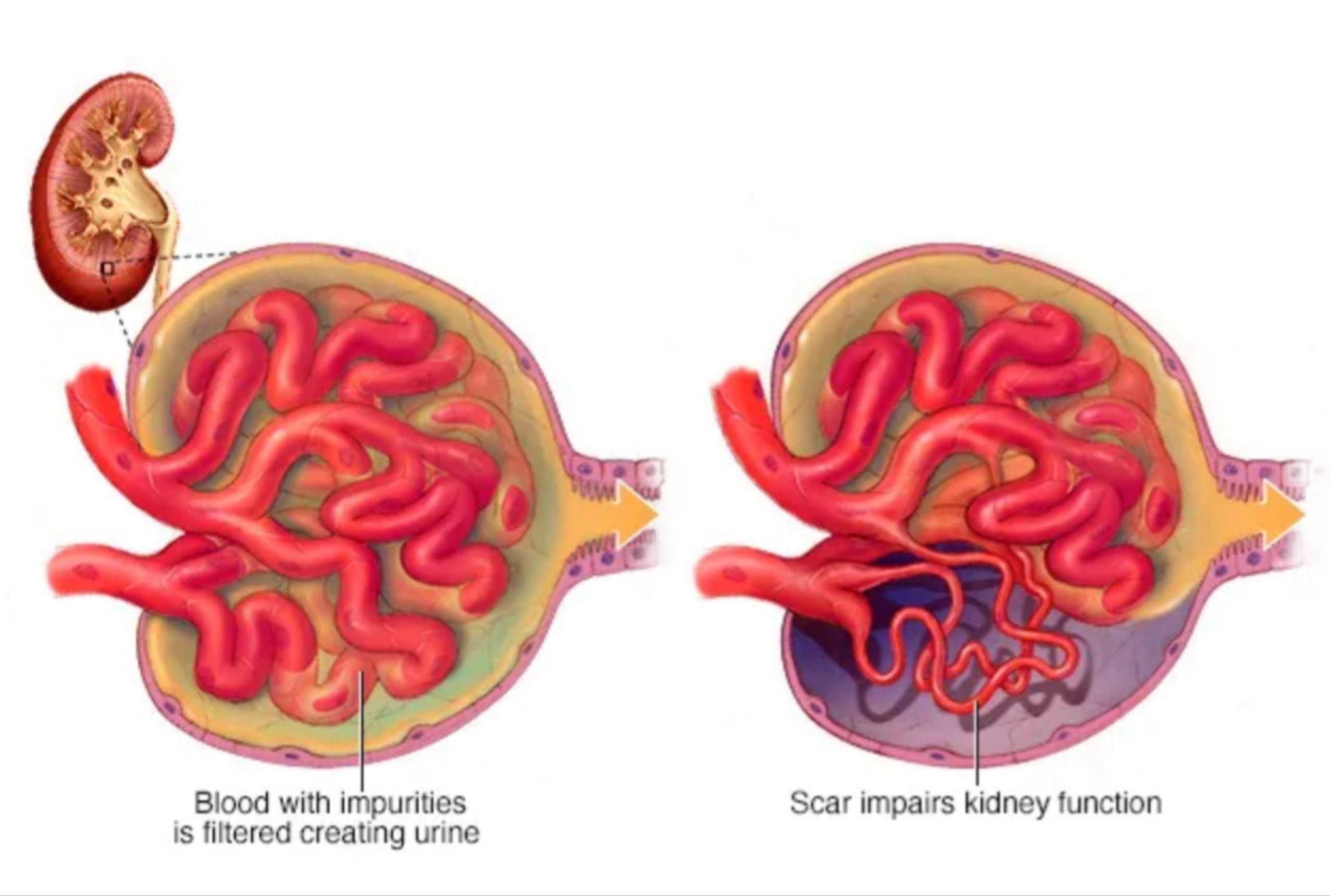
The most common kidney disease is focal segmental glomerulosclerosis, a chronic kidney disease that leads to the loss of nephron functionality, the main functional unit of the kidney whose purpose is to filter waste substances to eliminate them via urine.
The main analytes to consider are:
-Serum creatinine: Creatinine is a byproduct of muscle metabolism that is primarily eliminated through the kidneys.
Elevated levels of creatinine in the blood may indicate decreased renal function, especially if accompanied by low glomerular filtration, and it should be noted that the consumption of creatine monohydrate or other types of creatine increases the amount of creatinine, which is a waste product, and does not necessarily indicate kidney damage.
Normal values: 0.6 to 1.3 mg/dL in men and 0.5 to 1.1 mg/dL in women.
-Blood urea nitrogen (BUN): BUN is another marker of renal function. Elevated levels may indicate decreased renal function or dehydration, among other causes.
Normal values: 7 to 20 mg/dL.
-Estimated glomerular filtration rate (eGFR): It is an estimate of the glomerular filtration rate, that is, the rate at which the kidneys filter waste and excess fluid from the blood. It is calculated from serum creatinine, age, sex, and in some cases, race. A low eGFR may indicate decreased renal function.
Normal values: More than 90 mL/min/1.73m².
-Electrolytes (sodium, potassium, chloride, bicarbonate): Electrolyte levels may be altered in cases of kidney disease, and electrolyte imbalances can affect renal function.
-Serum sodium: Normal values: 135 to 145 mEq/L.
-Serum potassium: Normal values: 3.5 to 5.0 mEq/L.
-Serum chloride: Normal values: 96 to 106 mEq/L.
-Serum bicarbonate: Normal values: 22 to 29 mEq/L.
-Serum albumin: Albumin is a protein produced by the liver, and its level in the blood may decrease in cases of kidney disease, especially in advanced chronic kidney disease.
Normal values: 3.5 to 5.0 g/dL.
-Protein in urine (proteinuria): The presence of proteins in the urine may indicate damage to the glomeruli, as occurs in focal and segmental glomerulosclerosis.
Normal values: Less than 150 mg/day.
In addition, there are some additional coefficients that can provide even more information by cross-referencing data between different analytes:
-Estimated glomerular filtration rate (eGFR) with creatinine:
It is calculated using equations such as the MDRD (Modification of Diet in Renal Disease) equation or the CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration) equation, which take into account serum creatinine, age, sex, and in some cases, race.
Normal values: More than 90 mL/min/1.73m².
Desirable values: A high eGFR, indicating a good glomerular filtration rate and optimal renal function.
-Albumin-to-creatinine ratio (ACR):
It is a measure of the amount of albumin (a protein) in the urine relative to creatinine in the urine. It is used to detect and monitor proteinuria, which can be a sign of kidney damage.
Normal values: Less than 30 mg/g.
Desirable values: A low ACR, indicating minimal protein in the urine and normal renal function.
-BUN-to-creatinine ratio:
It is a ratio between blood urea nitrogen (BUN) and creatinine in the blood. It can help evaluate the cause of elevated creatinine, such as dehydration versus kidney disease.
Normal values: 10:1 to 20:1.
Desirable values: A BUN-to-creatinine ratio within the normal range, indicating normal renal function.
Additionally, there is another value that is the best predictor of renal damage, which is also complementary to the rest, and that is Cystatin C.
Cystatin C is a protein found in all cells that have a nucleus, and it is elevated when renal function is decreased. Furthermore, unlike other values, it is not influenced by the amount of muscle mass or protein intake in the diet.
Normal values are usually in the range of 0.5 to 1.1 mg/L.
9.Conclusion
As you can see, health is very important, and indeed, this is where the focus should be. A bodybuilder or a truly impressive physique is not built in 2 or 3 years, but in 10-15 years of work.
That's why it's crucial to be long-lived in this sport and not just live, but live with quality. That's why I see this type of information as necessary and accessible to anyone who wants to enjoy this lifestyle and, why not, the use of aids, which is a personal decision.
That's why I want to continue filling this blog with information for you, which by the way, is worth its weight in gold. 95% of coaches don't know about this, and they would really paya lot to know, but I think it's something you should have on hand and also be able to verify if the coach who is telling you how many anabolic steroids to inject into your body also knows how to foresee problems in time to solve them.
By the way, the best investment you can make is private health insurance, which costs around 40€ per month because with all the values needed for an analysis of a steroid user, it will cost you more than a kidney.
Remember that we are open to receiving content proposals for the blog and that prayers will be heard. Until the next article, greetings.
Nutribuilder
Julio
PED and Health Educator and Bodybuilding Contest Preparation Coach
